Connect With Us
Blog
Items filtered by date: March 2024
Lump in the Foot Arch and Plantar Fibroma
 Plantar fibroma is a benign condition characterized by the formation of a knot or nodule in the arch of the foot. This lump occurs in the plantar fascia, which is a thick band of tissue that runs from the heel to the toes. Typically, someone can feel it if they physically examine the foot. A plantar fibroma can develop in one or both feet, and it usually remains stable in size or grows slowly over time. The lump in the arch may or may not be painful. When pain is present, it's often because the fibroma presses against footwear or the ground, creating pressure on the foot. This discomfort can be increased by standing, walking, or wearing tight or unsupportive shoes. People sometimes modify their gait or posture in an attempt to minimize discomfort, which potentially causes secondary pain in the feet, legs, or back. Treatment options vary depending on the severity of symptoms. Conservative options may include orthotic devices and footwear modifications, and more invasive procedures may involve steroid injections or surgery. If you have a lump in the arch of the foot and suspect a plantar fibroma, it is suggested that you make an appointment with a podiatrist for diagnosis and treatment options.
Plantar fibroma is a benign condition characterized by the formation of a knot or nodule in the arch of the foot. This lump occurs in the plantar fascia, which is a thick band of tissue that runs from the heel to the toes. Typically, someone can feel it if they physically examine the foot. A plantar fibroma can develop in one or both feet, and it usually remains stable in size or grows slowly over time. The lump in the arch may or may not be painful. When pain is present, it's often because the fibroma presses against footwear or the ground, creating pressure on the foot. This discomfort can be increased by standing, walking, or wearing tight or unsupportive shoes. People sometimes modify their gait or posture in an attempt to minimize discomfort, which potentially causes secondary pain in the feet, legs, or back. Treatment options vary depending on the severity of symptoms. Conservative options may include orthotic devices and footwear modifications, and more invasive procedures may involve steroid injections or surgery. If you have a lump in the arch of the foot and suspect a plantar fibroma, it is suggested that you make an appointment with a podiatrist for diagnosis and treatment options.
A plantar fibroma may disrupt your daily activities. If you have any concerns, contact Gerald Erskine, DPM of Seneca Family Footcare. Our doctor can provide the care you need to keep you pain-free and on your feet.
Plantar Fibroma
A plantar fibroma is a fibrous knot in the arch of the foot. It is embedded in the plantar fascia which is a band of tissue that extends from the heel to the toes along the bottom of the foot. There can be multiple plantar fibromas in the feet at the same time. There are no known causes for this condition. If you have a plantar fibroma, there will be a bump in the arch of your foot that cannot be missed. Any associated pain is most often due to a shoe rubbing against the nodule. Non-surgical options, such as steroid injections, physical therapy, and orthotics should be tried first. Surgery is a last resort and is the only thing that will remove a plantar fibroma entirely. Consult with a podiatrist for a proper diagnosis and to determine the treatment regimen that is right for you.
What Causes a Plantar Fibroma?
While there are no specific causes identified, a plantar fibroma can possibly come from genetic predisposition or the formation of scar tissue that forms from healing the tears in the plantar fascia.
What Are the Symptoms of a Plantar Fibroma?
There will be a noticeable lump in the arch of the foot that may or may not cause pain. If pain is felt, it is typically because a shoe is rubbing up against the lump or when walking or standing barefoot.
Treatment and Prevention
A plantar fibroma will not disappear without treatment, but it can get smaller and be a non-issue. If pain persists, a podiatrist examines the foot and when the arch of the foot is pressed, pain can be felt down to the toes. An MRI or biopsy might be performed to help diagnose or evaluate the plantar fibroma. The following non-surgical options are generally enough to reduce the size and pain of these nodules:
- Steroid injections
- Orthotics
- Physical therapy to help apply anti-inflammatory creams on the bump
Surgery is considered if the mass increases in size and the patient continues to feel pain after non-surgical methods are tried.
If you have any questions please feel free to contact our office located in Ronceverte, WV . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Podiatrists Can Manage Cracked Heels

Cracked heels are a common foot condition characterized by fissures or splits in the skin, typically on the heels. They develop due to a combination of factors including dryness, pressure, and callus formation. Common causes include prolonged standing, wearing open-back shoes, obesity, and dry skin conditions like eczema or psoriasis. Besides being unattractive, cracked heels can become painful, especially if deep fissures form, leading to bleeding or infection risk. Calluses often accompany cracked heels, exacerbating discomfort. If left untreated, severe cases may lead to infections or difficulty while walking. Podiatrists are trained to diagnose and treat cracked heels effectively. They can remove thickened skin and calluses, offer advice on moisturizing and proper footwear, and address underlying conditions contributing to the problem. Additionally, they may recommend orthotic inserts to relieve pressure on the heels and prevent further cracking. If you have cracked heels that are painful or unsightly, it is suggested that you schedule an appointment with a podiatrist who can offer relief remedies.
If the skin on your feet starts to crack, you may want to see a podiatrist to find treatment. If you have any concerns, contact Gerald Erskine, DPM from Seneca Family Footcare. Our doctor can provide the care you need to keep you pain-free and on your feet.
Cracked Heels
It is important to moisturize your cracked heels in order to prevent pain, bleeding, and infection. The reason cracked heels form is because the skin on the foot is too dry to support the immense pressure placed on them. When the foot expands, the dry skin on the foot begins to split.
Ways to Help Heal Them
- Invest in a good foot cream
- Try Using Petroleum Jelly
- Ease up on Soaps
- Drink Plenty of Water
Ways to Prevent Cracked Heels
- Moisturize After Showering
- Skip a Shower
- Keep Shower Water Lukewarm
- Don’t Scrub Your Feet
If you are unsure how to proceed in treating cracked heels, seek guidance from a podiatrist. Your doctor will help you with any questions or information you may need.
If you have any questions, please feel free to contact our office located in Ronceverte, WV . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Achilles Tendon Pain

If you are experiencing pain in the back of your heel, you may have injured your Achilles tendon. This tendon, named after the legendary Greek warrior Achilles, connects the calf muscles to the heel bone. Achilles tendon injuries are common among athletes, particularly in sports like basketball and soccer. Symptoms include pain in the back of the heel or up the back of the leg, ranging from mild to severe. These injuries can occur in different places along the tendon, with the most serious being Achilles tendinopathy, which involves chronic inflammation and fluid buildup. Treatment typically involves rest, gentle stretching, and strengthening exercises. Prevention strategies include paying attention to foot mechanics, adjusting running stride, and building flexibility and strength in the lower legs through targeted exercises. If you are experiencing pain in your Achilles tendon area, it is suggested that you make an appointment with a podiatrist for an evaluation and treatment.
Achilles tendon injuries need immediate attention to avoid future complications. If you have any concerns, contact Gerald Erskine, DPM of Seneca Family Footcare. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is the Achilles Tendon?
The Achilles tendon is a tendon that connects the lower leg muscles and calf to the heel of the foot. It is the strongest tendon in the human body and is essential for making movement possible. Because this tendon is such an integral part of the body, any injuries to it can create immense difficulties and should immediately be presented to a doctor.
What Are the Symptoms of an Achilles Tendon Injury?
There are various types of injuries that can affect the Achilles tendon. The two most common injuries are Achilles tendinitis and ruptures of the tendon.
Achilles Tendinitis Symptoms
- Inflammation
- Dull to severe pain
- Increased blood flow to the tendon
- Thickening of the tendon
Rupture Symptoms
- Extreme pain and swelling in the foot
- Total immobility
Treatment and Prevention
Achilles tendon injuries are diagnosed by a thorough physical evaluation, which can include an MRI. Treatment involves rest, physical therapy, and in some cases, surgery. However, various preventative measures can be taken to avoid these injuries, such as:
- Thorough stretching of the tendon before and after exercise
- Strengthening exercises like calf raises, squats, leg curls, leg extensions, leg raises, lunges, and leg presses
If you have any questions please feel free to contact our office located in Ronceverte, WV . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
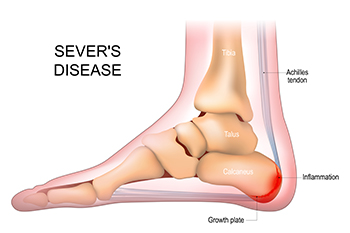
Gentle Stretches for Sever's Disease
Sever's disease, a common heel condition among active children, can cause discomfort, but incorporating gentle stretches into daily routines can offer relief. Targeting the calf muscles, a simple standing calf stretch involves placing the affected foot behind the other, pressing the heel into the ground. The soleus stretch, achieved by bending the knee while keeping the heel on the floor, targets the deeper calf muscles. Additionally, the seated hamstring stretch aids in maintaining flexibility in the lower leg. Gentle Achilles stretches, with a focus on controlled movements, can also contribute to easing the tension associated with Sever's disease. Incorporating these stretches into daily activities promotes flexibility and aids in managing discomfort. To prevent exacerbating symptoms, it is important to perform these exercises consistently and avoid overexertion. If your active child has heel pain, it is strongly suggested that you confer with a podiatrist who can diagnose and offer additional relief options.
Sever's disease often occurs in children and teens. If your child is experiencing foot or ankle pain, see Gerald Erskine, DPM from Seneca Family Footcare. Our doctor can treat your child’s foot and ankle needs.
Sever’s Disease
Sever’s disease is also known as calcaneal apophysitis, which is a medical condition that causes heel pain I none or both feet. The disease is known to affect children between the ages of 8 and 14.
Sever’s disease occurs when part of the child’s heel known as the growth plate (calcaneal epiphysis) is attached to the Achilles tendon. This area can suffer injury when the muscles and tendons of the growing foot do not keep pace with bone growth. Therefore, the constant pain which one experiences at the back of the heel will make the child unable to put any weight on the heel. The child is then forced to walk on their toes.
Symptoms
Acute pain – Pain associated with Sever’s disease is usually felt in the heel when the child engages in physical activity such as walking, jumping and or running.
Highly active – Children who are very active are among the most susceptible in experiencing Sever’s disease, because of the stress and tension placed on their feet.
If you have any questions, please feel free to contact our office located in Ronceverte, WV . We offer the newest diagnostic and treatment technologies for all your foot and ankle injuries.

